Improving cancer care in Norfolk: building personalised support in primary care
Over the past year, Norfolk Citizens Advice has been working in close partnership with Norfolk and Waveney Integrated Care Board (ICB) to strengthen the way people affected by cancer are supported within primary care.
This work focuses on one of the most critical yet often overlooked stages of the cancer journey: living with, and beyond, a cancer diagnosis. While clinical treatment often takes place in specialist settings, people frequently rely on their GP practice for ongoing support, reassurance and guidance long after treatment has finished.
At the centre of this programme is a specialist training and system support offer delivered across GP practices in Norfolk and Waveney. The programme equips both clinical and non‑clinical staff with the confidence, knowledge and skills needed to provide truly personalised cancer care, helping to ensure people receive the right support at the right time.
Why this work was needed
Earlier ICB‑supported research and system learning explored how well primary care teams felt equipped to support people affected by cancer. This work highlighted significant variation between GP practices.
It found that:
Many GP teams lacked confidence in supporting people following a cancer diagnosis, particularly once treatment had ended
There was often no clear or consistent pathway for follow‑up after end‑of‑treatment summaries were received from secondary care
People affected by cancer frequently described the move out of specialist services as a point when support dropped away abruptly
Non‑clinical barriers, including anxiety, low confidence, transport difficulties, financial pressures and wider social challenges, often delayed people accessing help or engaging fully with care
These findings made it clear that improving cancer care was not only about clinical treatment, but about strengthening personalised, practical and emotional support within primary care and the wider community.
Developing an evidence-led response
In response, Norfolk Citizens Advice, in partnership with the ICB, developed a programme designed to address these gaps by strengthening confidence, coordination and personalised follow‑up within primary care.
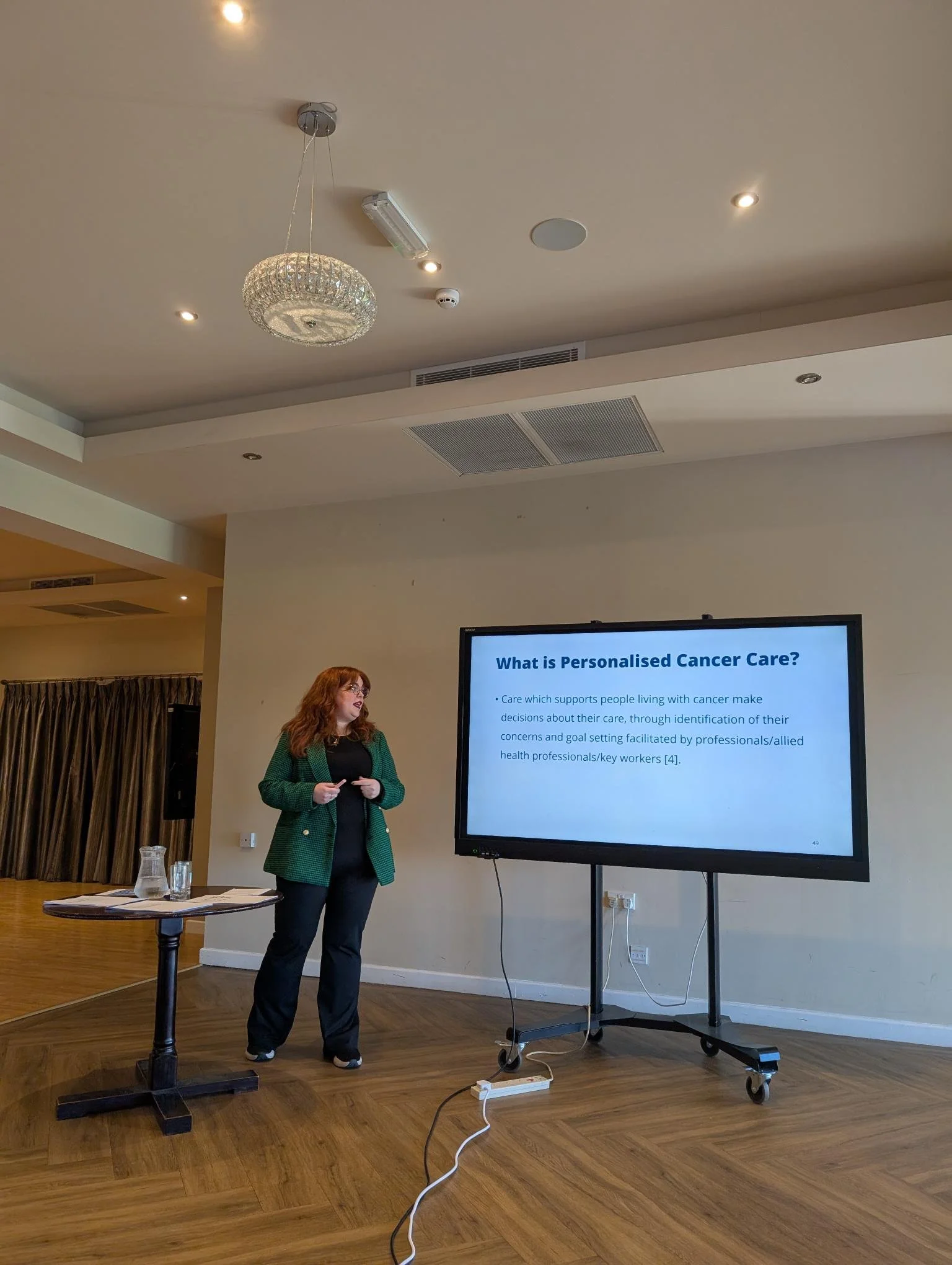
This work is led by Emma Chambers‑Ward, whose unique combination of clinical expertise, system knowledge and values‑driven practice has been central to its success.
About Emma Chambers-Ward
Emma is a Registered Nurse with over ten years’ experience across a range of healthcare settings, including older people’s medicine, respiratory, cardiology, gastroenterology, emergency care and primary care. She also brings extensive experience in healthcare assessment, motivational interviewing, coaching and leadership.
Throughout her career, personalised care has been at the heart of Emma’s practice. Her experience equips her with a rare blend of clinical insight, system understanding and strategic leadership, alongside a deep appreciation of the real‑world challenges faced by people affected by cancer.
Emma is particularly skilled at translating complex clinical concepts into practical, compassionate approaches that can be confidently used by both clinical and non‑clinical staff. Her work is grounded in national evidence, local system learning and a strong understanding of health inequalities.
Supporting earlier diagnosis and reducing inequalities
Beyond improving confidence and knowledge, this work supports wider system priorities by helping primary care teams recognise and address the non-clinical barriers that can delay help seeking, diagnosis and treatment.
By strengthening personalised conversations, improving navigation and understanding of services, and supporting people to overcome social barriers, the programme contributes to:
Earlier presentation with cancer concerns
Fewer missed or delayed appointments
Improved engagement with diagnostic pathways
More equitable access to care for people facing disadvantage, rural isolation or complex needs
This mirrors proven approaches used nationally, where trusted community and VCSE-led interventions have been shown to reduce delays, improve patient experience and support earlier diagnosis, particularly for groups most at risk of poorer outcomes.
Training the whole primary care team
Through this programme, Emma has designed and delivered training for GP practices across Norfolk and Waveney, supporting whole practice teams including reception staff, care co‑ordinators, social prescribing teams and clinicians.
The training supports staff to:
Deliver personalised cancer care that focuses on what matters most to each individual
Manage sensitive and difficult conversations with confidence
Understand health inequalities and barriers to access
Support people to navigate services and engage with care earlier
By improving confidence, knowledge and coordination across primary care teams, the programme reduces avoidable delays before, during and after key points in the cancer pathway. This supports more timely investigations, follow‑up and treatment.
Demonstrating clear impact
The results of the training programme have been consistently positive. Before taking part, staff reported relatively low baseline knowledge of personalised cancer care and low to moderate confidence in supporting people affected by cancer.
After training, there were clear and sustained improvements across all measures, with the largest gains seen in:
Knowledge of personalised cancer care
Practical confidence in real world conversations with patients
More than 90% of participants reported increased knowledge and confidence following the sessions.
Feedback from GP staff has been overwhelmingly positive, including:
“Articulate and well presented.”
“Fantastic course delivered by Emma, thoroughly well delivered”
“Good understanding of GP position in delivering cancer care”
“Emma is very knowledgeable and approachable.”
“The course was interactive, evidence based and left me feeling motivated to do more.”
“Excellent presentation and good training for holistic cancer management”
“For many years research has shown the importance of personalised care, and people affected by cancer have consistently reported they want to feel better supported by primary care, particularly after their treatment has finished. This training gives staff the confidence and skills to support people to live well beyond cancer. Importantly, personalised care principles apply across long term conditions, meaning the benefits extend far wider than cancer care alone”
Looking ahead
This programme demonstrates the value of strong partnerships between primary care, the voluntary and community sector and integrated care systems in delivering meaningful improvements in cancer support.
Continued investment would enable this evidence‑led approach to be expanded further across Norfolk, ensuring more GP practices and communities benefit from consistent, personalised cancer care. By embedding these skills across the system, more people can be supported effectively, inequalities reduced and outcomes improved.
Norfolk Citizens Advice is proud to be part of this work and remains committed to supporting people to get the right help, at the right time, through every stage of their cancer journey.